Have you been experiencing foot pain that worsens with standing or walking? You may be suffering from a condition known as Plantar Fasciitis. This article will provide an overview of common symptoms and diagnosis procedures for Plantar Fasciitis, so you can take the necessary steps to get relief.
So, let’s dive in to understand more about this painful condition.
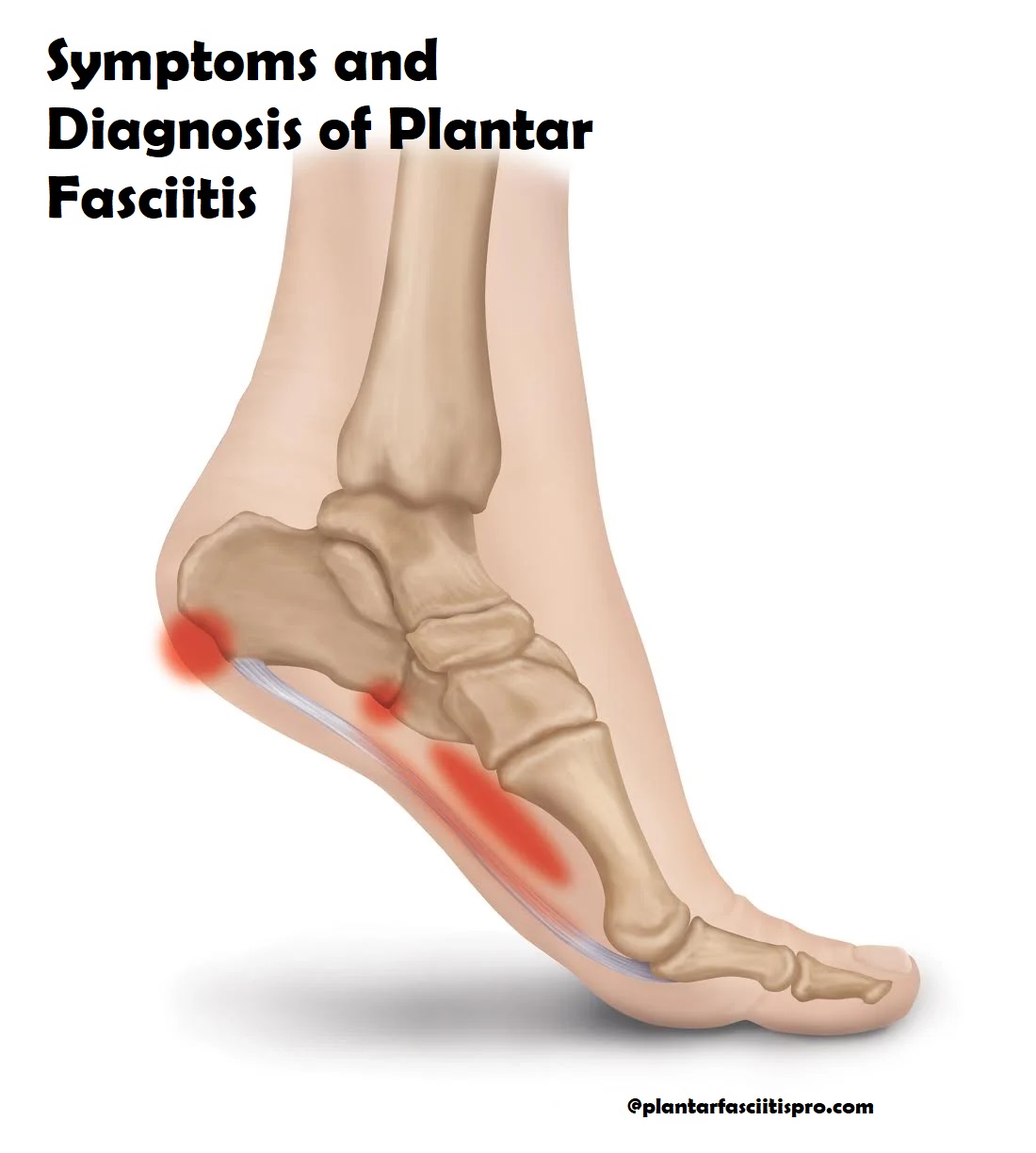
Plantar Fasciitis is a common foot disorder that is characterized by inflammation of the plantar fascia ligament, which connects the heel bone to the toes. It causes severe heel pain and discomfort, as well as difficulty in walking, running or any other physical activity. Additionally, patients often experience tightness and stiffness in their lower legs.
Plantar Fasciitis can occur due to a variety of reasons, including overuse or injury from high impact sports such as running and jumping. It may also be triggered by excessive strain on the feet due to poor-fitting shoes or incorrect body posture when standing for long periods of time. Other risk factors include being overweight, having flat feet and having weak foot muscles.
It is important to consult a doctor if you notice any signs or symptoms associated with Plantar Fasciitis in order to diagnose it accurately. Treatment options vary depending on the severity of the condition but generally focus on reducing pain and improving mobility via stretching exercises and bracing devices, orthotics or surgery in more severe cases.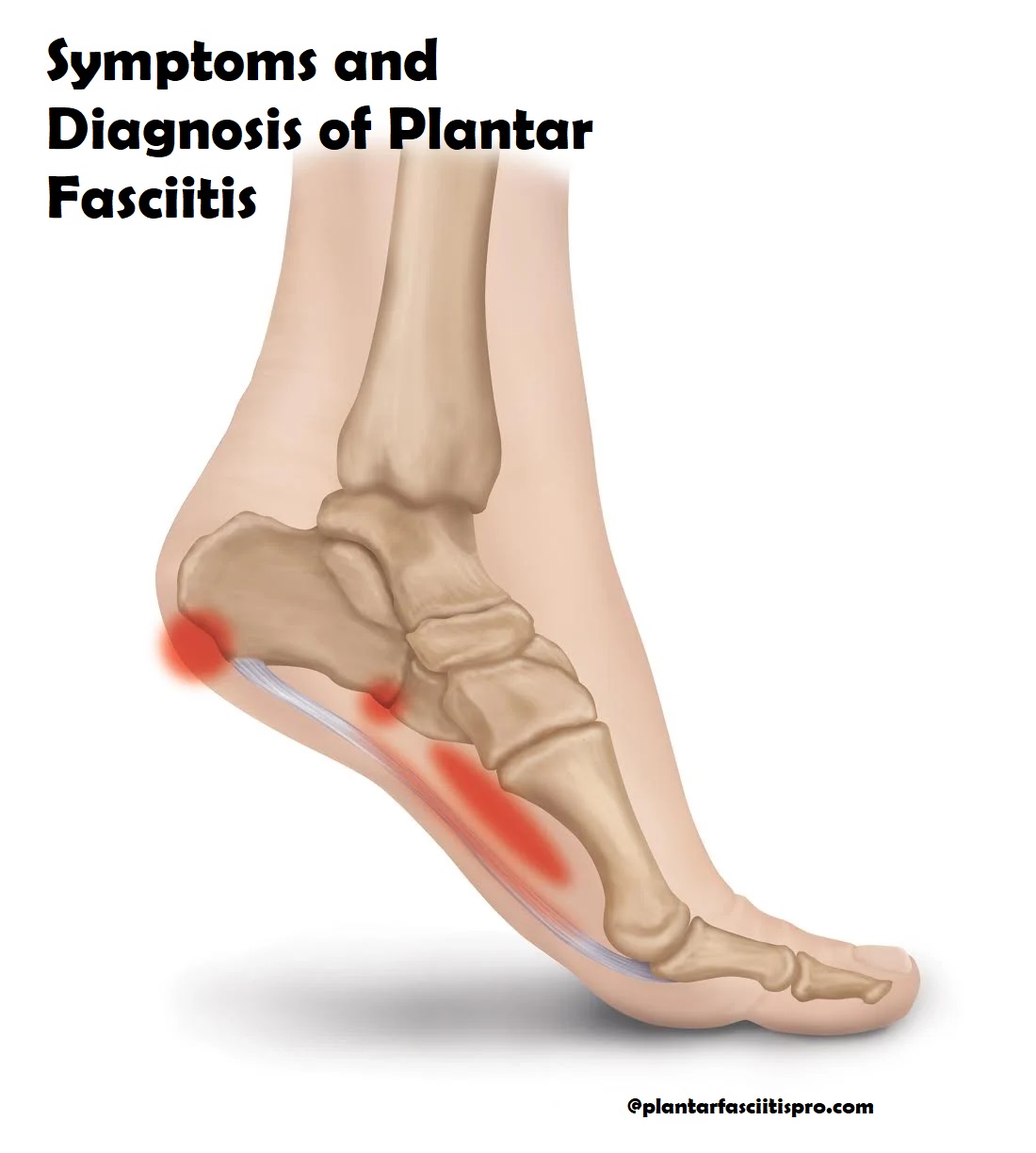
Definition of plantar fasciitis
Plantar fasciitis is a foot disorder that is best described as an inflammation of the plantar fascia, which is a thick band of connective tissue that stretches from the heel bone to the toes. Plantar fasciitis causes foot pain and may be worse after rest or when getting up in the morning. It typically affects people who put significant strain on their feet for various reasons—walking or running often, having high arched feet, wearing inappropriate shoes, having chronically tight calf muscles—all contribute to a greater risk of experiencing plantar fasciitis.
Although anyone can suffer from this condition, it is most common among middle-aged women and tends to occur in both feet. The most common symptom of plantar fasciitis is a sharp stabbing pain located between the heel and toes when first taking steps. This sensation usually diminishes as more steps are taken but may worsen after standing or walking for long periods of time. Other symptoms associated with plantar fasciitis include: pain along the arch of the foot; swelling at the heel; and tenderness along with limited flexibility in stretching certain muscles near the arch.
Symptoms of Plantar Fasciitis
Plantar fasciitis commonly causes pain located around the bottom of the heel or along the arch. This pain is often felt in the morning when taking your first steps after a long night of rest. The sensation may persist throughout day and worsen when standing for long periods of time, climbing stairs or walking on hard surfaces. Some people may even experience an increase in pain during the night that interrupts their sleep. For those who experience swelling on their feet, they may also notice a decrease in their range of motion.
It’s important to note that not everybody will have all the same symptoms, and it can vary case by case. However, some signs to watch out for include:
- Pain which is localized near the heel
- Discomfort that increases after activity or being on your feet for extended periods
- Swelling around where the injury has occurred
- Tenderness when pressure is applied directly to affected area
- Difficulty flexing foot due to limited range of motion
Pain in the heel
- Pain in the heel is the most common symptom of plantar fasciitis. The pain usually occurs in the inner or outer area of your heel with the pain increasing when you first stand and walk after a long period of rest, like when you wake up in the morning. Pain may also increase after activity or extended periods of standing.
Bending or stretching your foot so that your toes are pointed towards your shin can be very painful for those suffering from plantar fasciitis, as can walking on uneven surfaces. In some cases, even putting weight on your foot can be extremely painful and disabling.
Stiffness in the foot
Stiffness in the foot is a common symptom of plantar fasciitis. In some cases, the stiffness is so severe that it may cause difficulty or an inability to step without considerable pain or discomfort. Stiffness may also take the form of a sensation of tightness or pull in the arch, ankle, or Achilles tendon area. If left untreated, this stiffness can become worse and worsen other symptom areas.
To mitigate stiffness and other symptoms associated with plantar fasciitis, regular stretching exercises should be a part of any treatment program. Such stretches should focus on increasing flexibility in the calf muscles and through the arch area to help reduce foot tension an improve overall foot health. Additionally, footwear with arch support may also help reduce pain caused by strain on for the plantar fascia and prevent further tension in weakened structures of foot ligaments.
III. Differential Diagnosis
When diagnosing plantar fasciitis, a clinician must rule out other potential causes of heel pain. Differential diagnosis may consider joint diseases, nerve entrapment syndromes and biomechanical malalignment syndromes which could include the following:
-Achilles tendinitis
-Bursitis in the heel
-Stress fracture of the calcaneus
-Tarsal tunnel syndrome
-Arthritis in the foot or ankle joint
-Reactive (seronegative) arthritis/spondyloarthropathies
Other conditions may need to be ruled out to ensure that symptoms are accurately attributed to plantar fasciitis and not something else that may present with similar signs and symptoms. Imaging such as x-ray, magnetic resonance imaging (MRI) or ultrasound can help for accurate diagnosis of Plantar Fasciitis.
Heel spur
A heel spur is a calcium deposit that forms on the heel bone in people who have plantar fasciitis. Over time, these deposits can cause a bony protrusion at the bottom of the heel, known as a heel spur. Heel spurs may be visible on an X-ray, although they are often too small to be detected.
The presence of a heel spur does not necessarily indicate that it is causing pain. As such, many people with heel spurs do not experience any symptoms at all and only discover them incidentally during other diagnostics or examinations.
For those who do experience discomfort as a result of a heel spur, treatment typically involves stretching and/or wearing supportive shoes to help relieve pressure and pain in the affected area.
Tarsal tunnel syndrome
Tarsal tunnel syndrome is a nerve compression injury of the lower leg caused by a disorder of the tibial nerve, often associated with Plantar Fasciitis. This disorder is characterized by pain and/or paresthesia (tingling) in the plantar surface of the foot, radiating from the inside ankle bone. Pain or numbness may also be felt within or below the medial (inside) arch.
Diagnosis includes imaging in order to rule out any other medical conditions that could be causing the symptoms. It can also include manual evaluation, nerve conduction studies and EMG/NCS.
Treatment typically includes physical therapy, shoe orthotics and injections.
Physical Examination
The physical examination is an important part of diagnosing plantar fasciitis, as it helps the doctor or physical therapist to determine the extent of injury, as well as to rule out any other potential causes of pain. During a physical examination for plantar fasciitis, the doctor or therapist will take note of such things as the patient’s footwear, gait, posture, and range of motion. The patient will often be asked to do some exercises and movements designed to evaluate flexibility and strength in the feet and legs.
In a physical examination for plantar fasciitis, the primary goal is to identify any areas in which stress on the plantar fascia may be contributing to pain. This includes checking for tightness in both muscles and ligaments that are connected to or near the calf muscles (the gastrocnemius) and Achilles tendon (the soleus). The doctor may also palpate (or feel) specific areas along these structures while moving through different ranges of motion. They may also press down on certain points throughout these structures to pinpoint where pain is located. Other structures being assessed include foot arch height, arch flexibility, heel alignment and strength, toe mobility, midfoot mobility and stability of spine-hip-knee-ankle biomechanics.
Further evaluation may involve dynamic movements such as resisted dorsiflexion (toe up), inverted heel raises (inwardly rotating toes), heel walking (flexing your foot so only your toes touch floor when walking) single leg balance/maneuvers during standing or hopping tasks. Diagnostic imaging such as X-rays or MRI scans may also be necessary if there are signs that another condition might be present or if more detailed information about tissues within your foot is needed.
Palpation of the foot
- Palpation of the foot is an important step in the diagnosis of plantar fasciitis. This type of examination allows the provider to assess the tenderness and general condition of the plantar fascia along its full length. Palpation will typically determine tenderness to pressure over a specific point on the plantar fascia near its insertion point at the heel, as well as across the arch of the foot. The provider may also measure areas of edema or inflammation by gently pressing on certain points with their fingers or a finger-like object, such as a pen cap or other implement with a blunt and soft tip.
The examination should also include rotation and abduction-adduction tests that involve flexion and extension of the toes. This helps detect areas of thickening in response to strain related to activities such as running, jumping, and walking for long periods of time. The results can aid in confirming or ruling out possible causes for pain associated with plantar fasciitis and will help guide treatment recommendations going forward.
Range of motion testing
Range of motion testing is often used to diagnose plantar fasciitis. This type of testing involves taking measurements of how far you can move your foot with and without resistance from the doctor or from your own body weight.
First, the doctor will measure your range of motion (ROM) while you are standing and while you are lying flat on your back. Your ROM should be relatively the same in both positions. If it is not, this could be an indication that there is something wrong with the tissue in your foot which may be causing plantar fasciitis.
Next, the doctor will perform a series of tests designed to measure how well certain parts of your foot can move both on their own and when resistance is applied by either you or the doctor. Some tests measure flexibility while others measure strength and endurance. The most common tests involve having you bend your toes, stretch out your heel cord, hold a pointed position with your toes for a period of time, squat up and down from a seated position, or stand on one leg for a period of time without losing balance or dropping out of range.
All these tests should help indicate if there is an issue with any muscles or ligaments in the area around your feet which could be responsible for developing plantar fasciitis.
Imaging Tests
Imaging tests may be ordered to rule out other causes of foot pain such as a fracture or arthritis. X-rays, ultrasound and MRI scans can help in the diagnosis of plantar fasciitis. X-rays can show heel spurs, while an ultrasound or MRI image will display soft tissue damage better.
An ultrasound is less expensive and may be more available compared to an MRI. However, an MRI provides more detailed images and may provide a better view of certain structures (such as inflammations) within the foot.
X-rays
X-rays may be used to determine the cause and severity of the condition, as well as rule out other causes for heel, arch, or calf pain.
X-rays are an important tool in determining the cause of plantar fasciitis, and can identify calcium deposits or bony enlargements that may form with this condition.
In addition, they can provide information about any underlying medical conditions that might be affecting the ligament.
Ultrasound
Ultrasound imaging can be used to examine the condition of the plantar fascia, as well as any inflammation that may be present. During the ultrasound procedure, a handheld device is pressed against your foot, allowing sound waves to penetrate the tissues and create an image of what’s underneath your skin.
Ultrasound can also help to determine if any fluid has collected in the area due to inflammation. If this is the case, a doctor may recommend steroid injections. Additionally, with ultrasound imaging it is easier for doctors and physical therapists to determine which type of treatment might be most effective for your particular case of plantar fasciitis.
Conclusion
In conclusion, plantar fasciitis is an injury that can be very debilitating and it should be addressed as soon as possible so that chronic pain and disability can be avoided. As with most injuries, the best way to prevent plantar fasciitis is to take measures to avoid those activities that are known risk factors, such as running in worn-out shoes or standing on hard surfaces for long periods of time. If preventive measures are taken, the chances of developing this condition are significantly reduced.
If you do find yourself experiencing any of the symptoms associated with plantar fasciitis, it is important to seek medical attention right away. Diagnosis is usually quite straightforward and will involve a physical examination by a healthcare professional, along with imaging tests such as X-rays or MRI scans. Treatment for plantar fasciitis includes rest and physical therapy exercises, icing of inflamed areas, custom orthotics or arch supports, medications such as non-steroidal anti-inflammatory drugs (NSAIDs), and extracorporeal shock wave therapy (ESWT). Proper stretching prior to exercise is also essential in order to avoid this condition.
See Also-
- Best Hiking Boots For Plantar Fasciitis
- Best Golf Shoes Flantar Fasciitior
- Best Flip Flops for Plantar Fasciitis
- Best Dress Shoes For Plantar Fasciitis
- Best Crocs For Plantar Fasciitis